Tricipital reflex: what it is, physiology, and how it is analyzed
The neurological examination is, together with the anamnesis, the basis for the diagnosis of pathologies of the nervous system. Although many complex tests can be performed to assess muscle tone and intensity of contractions, one of the first steps when suspecting a problem at the level of the nervous system is always quantify tendon reflexes.
These reflexes are fast and involuntary, since they do not pass through the brain and are processed at the level of the spinal cord. Due to its variety and knowledge about them, it can be detected very precisely if any type of spinal cord damage, and if so, the injury can also be located very precisely. When the tendon reflexes are quantified, the force and speed of the contraction are measured, as well as the symmetry (or lack thereof) of the response and the homogeneity of the reaction between different parts of the Body.
In this type of test, it is not so important to put a number to each reflex from 1 to 5, but it is important to quantify the variability between the different neuronal sections and routes in the patient. Based on these interesting premises, we will tell you all about
the triceps reflex.- Related article: "Reflex arc: characteristics, types and functions"
What are tendon reflexes?
The tricipital reflex is a type of bone tendon reflex, so before we look at it, we must lay down some foundations in terms of medical terminology.
Tendon reflexes are a type of spinal reflex, whose route of action is extremely circumscribed and very fast. These types of actions do not pass directly through the brain, hence the speed of the association between the stimulus and the response.
When a force is applied to the critical point of the muscular environment, it is involuntarily lengthened. The neuromuscular spindle (sensory receptors within the muscle) then send the mechanical stress signal to an afferent neuron, which in turn comes into contact with the nerve center. The dorsal root ganglia pick up this stimulus, which is interpreted directly in the gray matter of the spinal cord. Finally, the axons of the motor neuron exit the spinal cord and send the muscle contraction signal.
As you can see, we are facing a very circumscribed closed circuit: spindle-afferent neuron-spinal cord-motor neuron. Because the information does not pass through the brain and is always interpreted at the same level, it is possible to detect neurological failures very accurately by quantifying the tendon reflexes. The most important are the following:
- Bicipital: it is investigated on the inner face of the elbow.
- Tricipital: consists of the percussion of the triceps.
- Radial-style: the styloid process of the radius is struck, into which the long supinator tendon is inserted.
- Ulna-pronator: percussion is performed at the level of the ulnar styloid.
- Patellar: the most famous of all. The patellar tendon is struck, causing an involuntary lifting of the leg.
- Achilles: the Achilles tendon is struck, which connects the calf muscle at the back of the leg with the heel bone.
What is the triceps reflex?
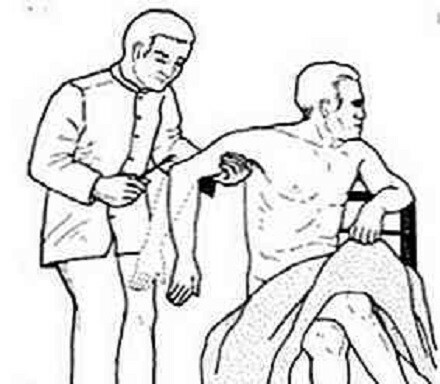
As we have said, the tricipital reflex is a type of osteotendinous reflex, and in turn myotatic, since the synaptic connection is made at the level of the spinal cord (and not the brain). To assess its functionality, a force is applied to the triceps tendon, located above the elbow (in the olecranon).. With this reflex, the C6, C7 (predominant) and C8 nerve roots come into play, or what is the same, the integrity of the musculocutaneous nerve.
To perform this test, the patient's forearm must be supported (ideally placed on the thigh), with the arm in a position that is midway between flexion and extension. Once the desired posture has been achieved, the triceps tendon must be located and percussed at its base of insertion.
When this sudden force is applied, the forearm is expected to extend rapidly. If the absence of movement is absolute (areflexia), myopathy, neuropathy, spondylosis, and other clinical entities of a neuromuscular nature are suspected.
How is it analyzed in patients?
In order to homogenize a test as subjective as this one, the National Institute of Neurological Disorders and Stroke devised a numerical scale applicable in all cases. Once the percussion occurs on the tendon of interest, the response is quantified based on the following parameters:
- 0: there is no answer, table considered as areflexia.
- 1: there is a reflex, but very little evident and less pronounced than normal. It includes a response trace or, failing that, a response that appears with reinforcement.
- 2: Reflex occurs, but is below the expected “half” or normal range.
- 3: Reflex occurs, above the expected “half” or normal range.
- 4: the reflex occurs, more than normal. Clonus, involuntary and rhythmic contractions of the muscular environment can appear after stimulation.
- 5 - Not always used, but this category may reflect sustained clonuses.
Depending on the rest of the answers, a triceps reflex between 2 and 3 can be considered "normal", as long as it occurs in the same way in both body planes (left and right arm). A value of 0 is conceived as areflexia, while a value 4-5 is hyperreflexia.
Furthermore, it should be noted that each of these values can be further circumscribed with a (+) or a (-), reflecting that the patient's table is between two of the figures. As you can imagine, a 3+ and a 4- can be the same for two different evaluators, so we repeat that the sign and the number are not as important as the homogeneity between results within the same patient.
- You may be interested in: "The 12 primitive reflexes of babies"
Interpretation of the results
An areflexia can show damage at the level of a particular nerve path or, failing that, an abnormality in the spine or the entire nervous system and general condition of the patient. Without going any further, some of the tendon reflexes are better predictors of diabetic neuropathy than many other subjective patient tests and symptoms.
On the other hand, hyperreflexia can indicate damage to the level of the upper motor neurons, whereas hyporeflexia or areflexia are usually indicative of motor neuron lesions lower. In general, a range 1+ to 3+ is estimated to be within normality if the response is symmetric. Anyway, even an absent reflex may be considered normal in some patients, if this is not accompanied by other symptoms and conditions that allow us to assume a problem at the neurological level.
Today, peripheral neuropathies are the most common cause of absence of reflexes in general society. The triggers of this condition are very varied: diabetes, alcoholism, amyloidosis, uremia, deficiencies vitamins, pernicious anemia, remote cancer, presence of toxins in the body and many other agents etiological. Once an abnormality is detected in the tricipital reflex (or any bone tendon reflex), it is time to go to more tests until the patient's problem is found.
Summary and final notes
As you may have seen, the triceps reflex (and the tendon reflexes in general) is essential. for clinical semiology, especially when detecting peripheral nervous system neuropathy. These reflexes are very important in the medical field, because by not "passing" through the brain, it is possible to clearly detect the damage in a very specific environment to the involved section of the spinal cord spinal.
Thus, reflexes are very useful when it comes to detecting pathologies, but they must be accompanied by a series of accessory tests to confirm or rule out a diagnosis. Osteotendinous reflexes are the first step in suspecting a disease, but they never alone make up the complete diagnosis.