Discover what the BONE FORMATION is like
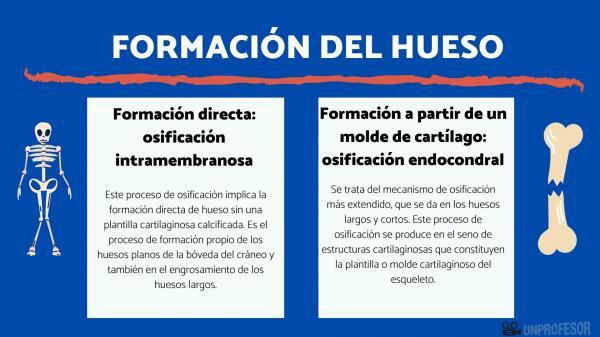
The bone tissue formation it takes place through two ossification mechanisms. Although bones Formed by one mechanism or another, they are indistinguishable in structure and biomechanical properties. In this lesson from a TEACHER we will see in detail which are the two mechanisms of bone formation.
East ossification process implies the direct bone formation without a calcified cartilaginous template. It is the formation process of the flat bones of the skull vault and also in the thickening of the long bones.
Intramembranous ossification occurs in the mesenchyme (embryonic connective tissue, with a supporting function that fills the space between cells and organs) or, in more advanced stages of development, in the periosteum (connective tissue that surrounds the bones that differentiates from the mesenchyme).
The intramembranous ossification process takes place in the following steps:
- Vascularization of the mesenchyme: In a first stage, an increase in the vascularization of this tissue is observed; due to the differentiation of some cells of the mesenchyme, into cells of the blood vessels.
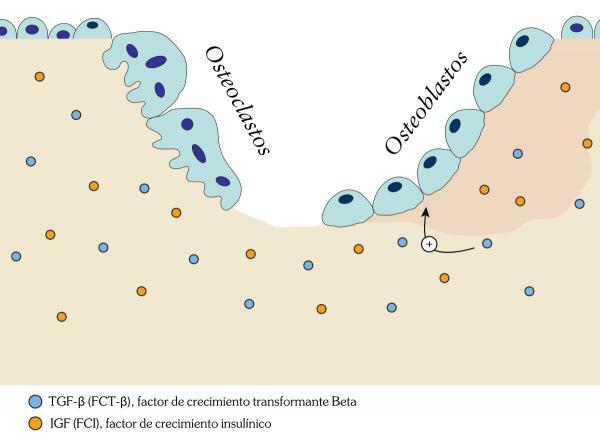
- Proliferation of osteoblasts: Then other cells in the mesenchyme become osteoblasts. The osteoblasts They are the cells of bone tissue, which are responsible for producing an extracellular matrix composed of collagen and proteoglycans.
- Ossification: Once this extracellular matrix is constituted, the osteoblasts capture calcium from the bloodstream of the mother and deposit it in the extracellular matrix in the form of calcium carbonate crystals (hydroxyapatite). Hydroxyapatite hardens the extracellular matrix forming bone tissue. When this happens, the osteoblast ceases its activity and becomes an osteocyte. The osteocytes They are the cells of the bone tissue in charge of providing the necessary nutrients to the matrix.
It is the most widespread ossification mechanism, which occurs in long and short bones. This ossification process occurs within the cartilaginous structures that constitute the cartilaginous template or mold of the skeleton.
This mold is formed by hyaline cartilaginous tissue (hard connective tissue) and mesenchyme. This bone skeleton hammer already presents its characteristic shape after six weeks of embryonic development. The cartilaginous outline or mold is formed by osteocytes and a gelatinous extracellular matrix formed by proteoglycans, glycoproteins, collagen fibers and water.
This process consists of the following steps:
1. Chondrocyte proliferation and bone collar formation
- Around the seventh week of embryonic development, chondrocytes multiply in the cartilaginous mold that will give rise to bone.
- Chondrocytes are cells of the cartilage tissue that originate from the differentiation of chondroblasts, which are cells of the mesenchyme.
- At a certain point, the chondrocytes in the central part stop dividing and a bony collar is created that is generated by the osteoblasts on the cartilage surface. This ring serves as a support for the bone in formation.
2. Chondrocyte hypertrophy
Once the bone collar is formed, the chondrocytes that have been locked inside it greatly increase in volume. This is due to the increase in the amount of organelles involved in the synthesis, distribution and secretion of biomolecules (endoplasmic reticulum, Golgi complex and secretion vesicles).
In this stage the chondrocytes synthesize and secrete large amounts of collagen and elastic fibers. Chondrocytes occur in small groups and are surrounded by a thin layer of extracellular matrix that is different from cartilage matrix. The set of this matrix and the group of chondrocytes is called chondron or chondroma.
3. Extracellular matrix mineralization
Chondrocytes secrete large amounts of calcium that are deposited in the extracellular matrix in the form of crystals of calcium phosphate.
4. Apoptosis
The calcification of the matrix causes the death of chondrocytes (apoptosis or programmed death), which become isolated and stop receiving nutrients.
5. Vascular invasion
From the eighth week, the blood capillaries invade the calcified matrix and osteogenic cells (undifferentiated cells that will give rise to different types of cells) occupy the place left by the osteocyte.
6. Ossification
Osteogenic cells differentiate giving rise to osteoblasts, responsible for generating the bone matrix. Osteoblasts produce bone matrix from previously calcified cartilage. As a result of the process, the first bone trabeculae (small partitions that form a network with large empty spaces inside), which have a central axis formed by cartilage. Creating the primary spongy tissue or fibrillar. This spongy tissue is an immature and poorly organized tissue in which the collagen fibers do not present a lamellar distribution, but are presented in a cross-linked manner.
7. Lamellar bone remodeling
- At the same time that the deposition of calcium in the form of hydroxyapatite continues, the chondroclasts (cells responsible for the destruction of cartilage) remove the calcified cartilage from the matrix, in a rhythmic way with the formation of bone.
- In this process of bone maturation, two types of bone tissue can be formed that are characterized by their concentric laminated structure. According to its characteristics it differs:
- The spongy or secondary laminar tissue It presents an organization defined in concentric layers formed by trabeculae.
The cortical or compact tissue which occupies the most peripheral part formed in this case by concentric flat sheets around a channel (Harvers canal) through which blood vessels and nerves pass.
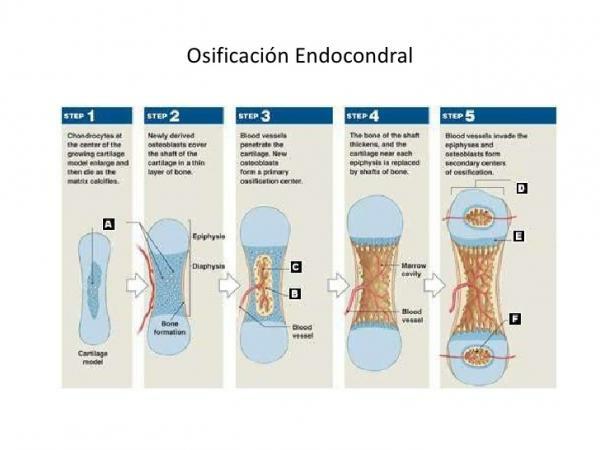
To finish this lesson on bone formation, we are going to talk about the endochondral ossification process that occurs, first of all, in the primary center of ossification, in the middle part of the bone (diaphysis) and, later, secondary centers of ossification are generated at the ends of this (epiphysis).
Primary center of ossification
From the seventh week of embryonic development, ossification of the long bones begins from the primary center of ossification, which is located in the diaphysis (intermediate part of the bone).
As time passes, the osteoblasts migrate towards the ends of the bone (epiphysis) creating the growth cartilage, which produces the longitudinal growth of the bone.
In addition, there is a slight increase in bone thickness (diameter), due to the formation of tissue by part of the periosteum that generates bone by intramembranous ossification from the outside to the inside of the bone
Secondary centers of ossification
At birth, all the diaphyses are ossified while the epiphyses are cartilaginous.
Ossification in the secondary centers occurs after birth. The formation of secondary ossification centers occurs in the later stages of embryonic development in the epiphyses of the bone. The secondary centers of ossification are called growth plates or epiphyseal.
These centers of ossification grow from the inside towards the periphery of the bone. In the growth plates there is the formation of cancellous bone (formed by trabeculae) that lacks periosteum (dense and thin membrane that covers the bones and contains the nerves and blood vessels that nourish the bone).
Image source: CK12